Vaccination is one of the major success stories of modern medicine, greatly reducing the incidence of infectious diseases. (measles, and eradicating others, such as smallpox). Conventional vaccine approaches have not been as effective against rapidly evolving pathogens like influenza or emerging disease threats such as the Ebola or Zika viruses.
RNA-based vaccines could have an impact in these areas due to their shorter manufacturing times and greater effectiveness. Beyond infectious diseases, RNA vaccines have the potential as novel therapeutic options for major diseases such as cancer. The mRNA vaccine field is developing extremely rapidly; A large body of preclinical data has accumulated over the past several years, and multiple human clinical trials have been initiated. COVID-19 mRNA vaccines give instructions for our cells to make a harmless piece of what is called the “spike protein.”
KEY POINTS ABOUT RNA-VACCINES
- Unlike a normal vaccine, RNA vaccines work by introducing an mRNA sequence (the molecule which tells cells what to build). The mRNA sequence is coded for a disease-specific antigen. Once produced within the body, the antigen is recognized by the immune system, preparing it to fight the real thing.
- RNA vaccines are faster and cheaper to produce than traditional vaccines. An RNA-based vaccine is also safer for the patient, as it is not produced using infectious elements.
- Production of RNA vaccines is laboratory-based, and the process could be standardized and scaled, allowing quick responses to large outbreaks and epidemics
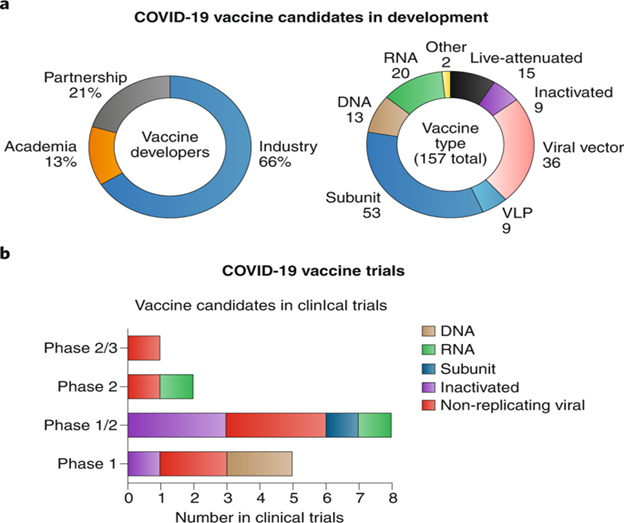
- Most current research is into RNA vaccines for infectious diseases and cancer, for which there are several early-stage clinical trials, there is also some early research into the potential of RNA vaccines for allergies
- There is still a lot of work to be done before mRNA vaccines can become standard treatments, in the meantime, we need a better understanding of their potential side effects, and more evidence of their long-term efficacy.
Conventional vaccines usually contain inactivated disease-causing organisms or proteins made by the pathogen (antigens), which work by mimicking the infectious agent. They stimulate the body’s immune response, so it is primed to respond more rapidly and effectively if exposed to the infectious agent in the future.
RNA vaccines use a different approach that takes advantage of the process that cells use to make proteins: cells use DNA as the template to make messenger RNA (mRNA) molecules, which are then translated to build proteins. An RNA vaccine consists of an mRNA strand that codes for a disease-specific antigen. Once the mRNA strand in the vaccine is inside the body’s cells, the cells use the genetic information to produce the antigen. This antigen is then displayed on the cell surface, where it is recognized by the immune system.
- Basic Principle and Procedure of Fungal Staining
- What are Oxygen absorbers and How works?
- What is Pasteurization?
- What is Disinfectant and antiseptic? Disinfectants vs antiseptic
- Why More Men are Dying from Coronavirus than Women?
How are RNA vaccines produced?
A major advantage of RNA vaccines is that RNA can be produced in the laboratory from a DNA template using readily available materials, less expensively and faster than conventional vaccine production, which can require the use of chicken eggs or other mammalian cells.
RNA vaccines can be delivered using a few methods: via needle-syringe injections or needle-free into the skin; via injection into the blood, muscle, lymph node, or directly into organs; or via a nasal spray. The optimal route for vaccine delivery is not yet known. The exact manufacturing and delivery process of RNA vaccines can vary depending on the type.
Types of RNA vaccine
Non-replicating mRNA vaccines
The simplest type of RNA vaccine, an mRNA strand is packaged and delivered to the body, where it is taken up by the body’s cells to make the antigen.
In vivo self-replicating mRNA
The pathogen-mRNA strand is packaged with additional RNA strands that ensure it will be copied once the vaccine is inside a cell. This means that greater quantities of the antigen are made from a smaller amount of vaccine, helping to ensure a more robust immune response.
In vitro dendritic cell non-replicating mRNA vaccines
Dendritic cells are immune cells that can present antigens on their cell surface to other types of immune cells to help stimulate an immune response. These cells are extracted from the patient’s blood, transfected with the RNA vaccine. Then gave back to the patient to stimulate an immune reaction.
ADVANTAGES OF mRNA vaccines
- Safety: RNA vaccines are not made with pathogen particles or inactivated pathogen, so are non-infectious. RNA does not integrate itself into the host genome. The RNA strand in the vaccine is degraded once the protein is made.
- Efficacy: Early clinical trial results indicate that these vaccines generate a reliable immune response. Vaccines (mRNA) are well-tolerated by healthy individuals, with few side effects.
- Production: vaccines can be produced more rapidly in the laboratory in a process that can be standardized, which improves responsiveness to emerging outbreaks.
challenges
The methods to make mRNA vaccines can be very effective. However, there are technical challenges to overcome to ensure these vaccines work appropriately:
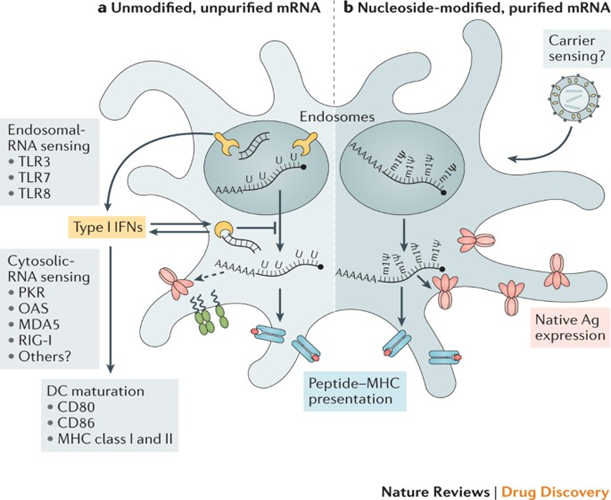
- Unintended effects: the mRNA strand in the vaccine may elicit an unintended immune reaction. To minimize this the mRNA vaccine sequences are designed to mimic those produced by mammalian cells.
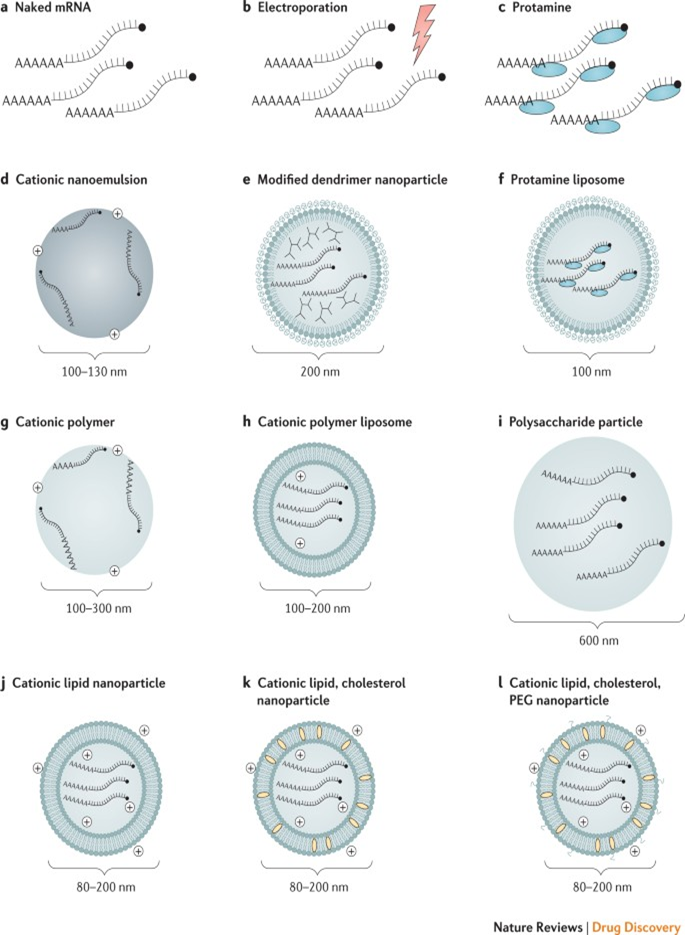
- Delivery: delivering the vaccine effectively to cells is challenging since free RNA in the body is quickly broken down. To help achieve delivery, the RNA strand is incorporated into a larger molecule to help stabilize it and/or packaged into particles or liposomes.
- Storage: many RNA vaccines, like conventional vaccines, need to be frozen or refrigerated. Work is ongoing to reliably produce vaccines that can be stored outside the cold chain since these will be much more suitable for use in countries with limited or no refrigeration facilities.
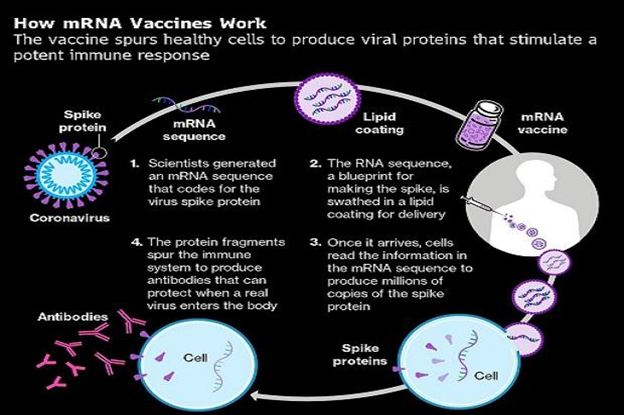
A Closer Look at How COVID-19 mRNA Vaccines Work
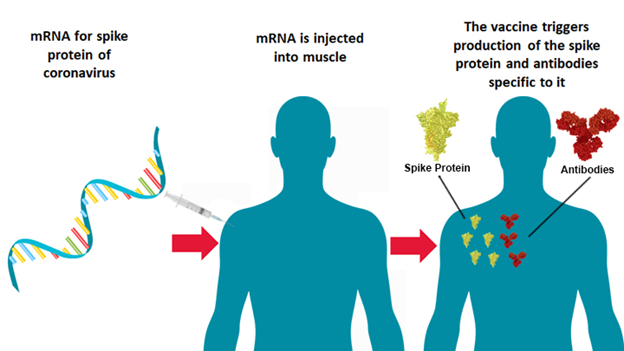
COVID-19 mRNA vaccines give instructions for our cells to make a harmless piece of what is called the “spike protein “. The spike protein is found on the surface of the virus that causes COVID-19.
COVID-19 mRNA vaccines are given in the upper arm muscle. Once the instructions (mRNA) are inside the immune cells, the cells use them to make the protein piece. After the protein piece is made, the cell breaks down the instructions and gets rid of them.
Next, the cell displays the protein piece on its surface. Our immune systems recognize that the protein does not belong there and begin building an immune response and making antibodies, like what happens in natural infection against COVID-19.
At the end of the process, our bodies have learned how to protect against future infection. The benefit of mRNA vaccines, like all vaccines, is those vaccinated gain this protection without ever having to risk the serious consequences of getting sick with COVID-19.
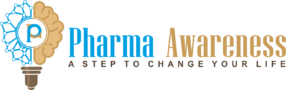
Progress in mRNA vaccines delivery
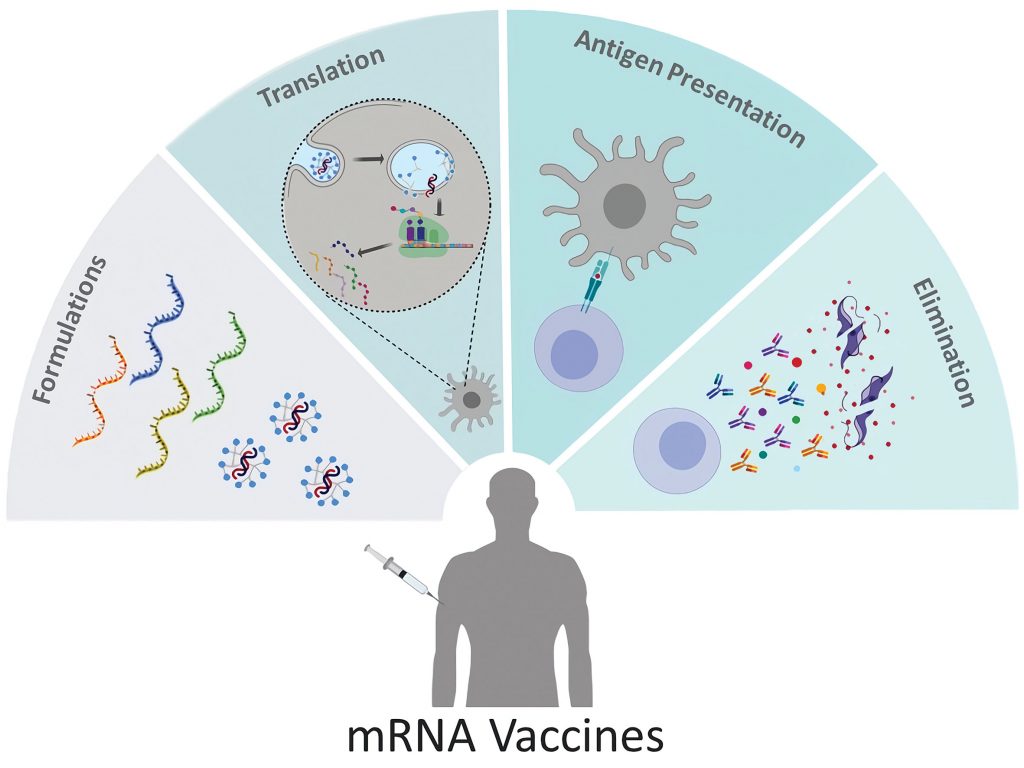
Efficient mRNA delivery is critical to achieving therapeutic relevance. Exogenous mRNA must penetrate the barrier of the lipid membrane in order to reach the cytoplasm to be translated into a functional protein. mRNA uptake mechanisms seem to be cell type-dependent, and the physicochemical properties of the mRNA complexes can profoundly influence cellular delivery and organ distribution. There are two basic approaches for the delivery of mRNA vaccines that have been described to date. First, the loading of mRNA into DCs ex vivo, followed by re-infusion of the transfected cells. Second, direct parenteral injection of mRNA with or without a carrier.
DC loading allows precise control of the cellular target, transfection efficiency. The other cellular conditions, but as a form of cell therapy, it is an expensive and labor-intensive approach to vaccination. Direct injection of mRNA is comparatively rapid and cost-effective. But it does not yet allow precise and efficient cell-type-specific delivery, although there has been recent progress in this regard. Both of these approaches explored in a variety of forms.
CONCLUSION
Researchers have been studying and working with mRNA vaccines for decades. Interest has grown in these vaccines because they can be developed in a laboratory using readily available materials. This means the process can be standardized and scaled up, making vaccine development faster than traditional methods of making vaccines.
mRNA vaccines have been studied before for flu, Zika, rabies, and cytomegalovirus (CMV). As soon as the necessary information about the virus that causes COVID-19 was available, scientists began designing the mRNA instructions for cells to build the unique spike protein into an mRNA vaccine.
Future mRNA vaccine technology may allow for one vaccine to provide protection for multiple diseases. Thus decreasing the number of shots needed for protection against common vaccine-preventable diseases. Vaccines (mRNA) represent a promising alternative to conventional vaccine approaches because of their high potency, capacity for rapid development, and potential for low-cost manufacture and safe administration. However, their application has until recently been restricted by the instability and inefficient in vivo delivery of mRNA.
Recent technological advances have now largely overcome these issues and multiple mRNA vaccine platforms against infectious diseases. Several types of cancer have demonstrated encouraging results in both animal models and humans. This Review provides a detailed overview of mRNA vaccines and considers future directions and challenges in advancing this promising vaccine platform to widespread therapeutic use.
Author:
- Ransh Pharma: Best Intermediates Manufacturing Unit at Visakhapatnam
- What is 3D Bioprinting? Basic Principles, Techniques, and Application of 3D Bioprinting.
- Basic Principle and Procedure of Fungal Staining
- OXYGEN MANAGEMENT FOR SUSTAINABLE ENVIRONMENT
- mRNA VACCINES FOR COVID-19
- LITHIUM-ION BATTERIES An idea towards energy sustainability
- Artificial Leaf – A Blessing for Energy Crisis
- What are Oxygen absorbers and How works?
- What is Pasteurization?
- What is Disinfectant and antiseptic? Disinfectants vs antiseptic
- Why More Men are Dying from Coronavirus than Women?
- HOW COVID-19 SPREADS?
- What are the COVID-19 Symptoms?
- What is Coronavirus? How Coronavirus can Enter into our Body?
- Telemedicine Industry Analysis of Key Trends and Drivers Shaping Future Growth
- Rising Prevalence of Adverse Drug Reactions Drives Global Market for Pharmacovigilance
- Common Pharma Abbreviations
- Bioremediation : Promise for Eco-friendly enact|What is Bioremediation?
- GENERAL PROCEDURE FOR PASSIVATION
- How the New Drug approval process of CDSCO works?
- What is Passivation? How Does Passivation Process Work? How to Passivate Stainless Steel Parts?
- Explore new openings in Pharma Profession by Making yourself Skilled as Technical Associate in The Central Drugs Standard Control Organisation CDSCO
- What is Data Integrity and ALCOA Plus
- GOWNING PROCEDURE IN CLEAN ROOM
- How to Crack Your Job Interview?
- 10-Deacetylbaccatins (10 DAB) NATURAL ORGANIC COMPOUNDS USED AS STARTING MATERIAL FOR ANTICANCER DRUGS PRODUCTION
- Difference between C8 and C18 Columns Used in HPLC System
- KNOW ABOUT TOTAL QUALITY MANAGEMENT AND CURRENT GOOD MANUFACTURING PRACTICES (cGMP)